Autism Spectrum Disorder (ASD) is a group of brain development disorders defined by stereotypical behavior with communication and social interaction deficiencies. In 2012, the incidence of this disorder was estimated at 14.6 per 1000 children aged 4.24
To date, the exact causes of ASD haven’t been fully understood and the available treatment methods are very limited. Previous studies focused in particular on investigating the role of genetic causes, immune system dysregulation, inflammation, the impact of toxic substances and intestinal microbiota.
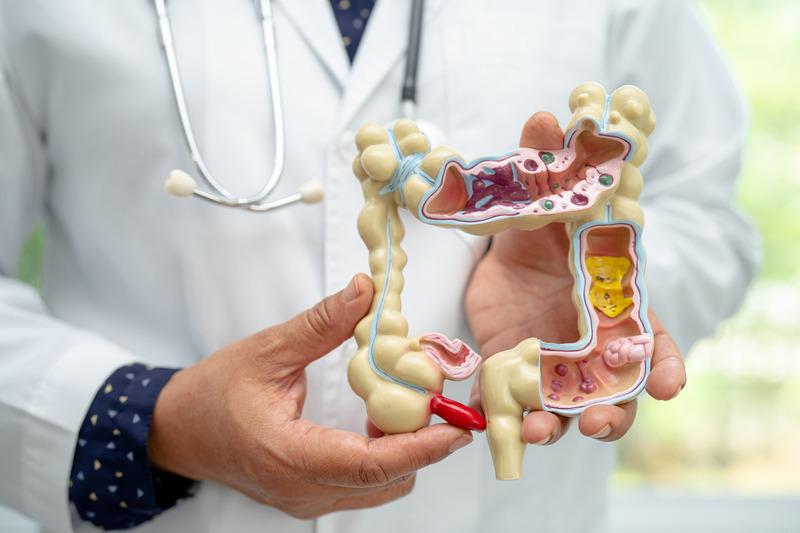
Clinical findings indicate that gastrointestinal symptoms such as abdominal pain, flatulence, diarrhoea or constipation occur in patients with ASD much more frequently than in the rest of the population. Additionally, it was found that children with ASD who also suffer from gastrointestinal problems score worse when it comes to typical ASD symptoms such as mood swings, hyperactivity, and socialization/communication deficiencies.25,26 Therefore, the treatment of GI symptoms in children with ASD is receiving ever more attention.
Several clinical studies have demonstrated that the composition of intestinal flora in autistic patients differs significantly compared to healthy populations. For example it been found that patients with ASD suffering from constipation have an increased presence of particular strains of bacteria such as Escherichia / Shigella and Clostridium in the gut. On the contrary, other bacterial strains are often under-represented.27
Currently, research is focusing on the use of FMT in the treatment of ASD based on the assumption that FMT can normalize intestinal microbiota in these patients and reduce GI symptoms.28
A recent clinical trial conducted in 2017 confirmed this hypothesis in practice. FMT therapy was administered to 18 children with ASD aged 7 to 16 years. All children also suffered from gastrointestinal symptoms. The results of the study showed that after treatment, gastrointestinal symptoms such as constipation, diarrhoea and abdominal pain were reduced on average by 80%. More surprising, however, was the finding that there was a significant reduction in ASD-related symptoms in children after FMT, such as moodiness, hyperactivity, lethargy, stereotypical behaviour, and speech/communication problems. As a result, the mean development age (measured on the VABS-II clinical scale) in these children increased by 1.4 years after FMT and these positive changes persisted even 2 months after treatment.28
Despite the very positive results of this pilot study, it is worth mentioning that the use of FMT therapy in children with ASD is a completely new concept and falls under experimental treatment. Other clinical trials are necessary to confirm the efficacy of FMT in ASD patients, particularly in children without digestive problems.

 SK
SK